What is Visual Snow Syndrome?
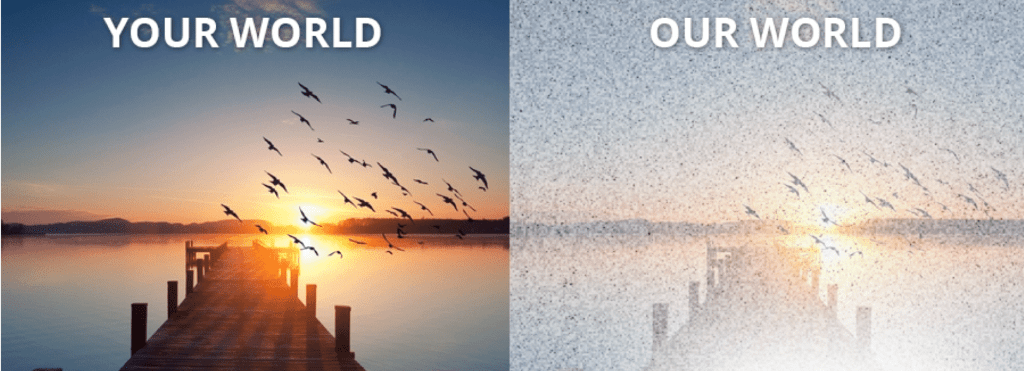
Visual Snow Syndrome (VSS) is a neurological disorder that impacts an individual’s vision, hearing, cognition, sensory processing, and quality of life. The brain of an individual with VSS processes visual information abnormally, as well as other sensory information. Visual Snow (VS), is the primary symptom of the condition of which it is also named after. VS entails seeing snow-like static throughout the entire visual field (with your eyes open and closed). However, the condition also encompasses an array of other debilitating visual and non-visual symptoms. VSS symptoms impact an estimated 2-3% of the world’s population. People of all ages and backgrounds worldwide are affected by VSS daily. Some experience symptoms since birth while others experience the sudden onset of the condition.
Researchers have identified measurable differences in the brains of those with VSS. They have increased metabolic activity, especially in areas involved in visual perception and processing. VSS is linked to abnormalities in serotoninergic (serotonin) and glutamatergic (glutamate) neurotransmission. Factors that impact the nervous system and induce neurotransmitter alterations, neuroplasticity, or structural and functional changes within the brain have the potential to affect the intensity of VSS symptoms. Data has also shown that VSS symptoms are not a manifestation of anxiety and depression; instead, the debilitating nature of these symptoms coupled with the medical community’s historic marginalization, misdiagnosis, and mistreatment of VSS patients can have a profound, devastating impact on their mental health.
Evidence has now proven that VSS is a legitimate and distinct neurological condition that entails both visual and non-visual symptoms. As more information about the condition is discovered and reports of VSS continue to rise, it is gaining increased medical and scientific recognition globally.
Additional awareness, education, resources, and research are needed to help the millions of people who are affected by VSS. Collective advocacy efforts will allow the world to become more informed about the condition, ensuring a timely diagnosis for patients, increased support, further understanding regarding VSS, continued treatment development, and a potential cure for the disorder.
For more information about VSS, please review the sections and resources below.
Symptoms of VSS
The primary symptom of VSS is seeing visual snow, which can be described as seeing static, flickering dots, and flashing lights 24/7 (with your eyes open and closed). Some describe it as trying to see in the middle of a snowstorm or through a snow globe that has been shaken up. However, VSS entails more than just seeing visual snow. People with VSS also commonly experience many other debilitating visual and non-visual symptoms, such as palinopsia, photophobia, tinnitus, paresthesia, anxiety, depression, depersonalization, and insomnia. The intensity, appearance, and degree of impact of these symptoms range from mild to moderate to life-altering, depending on the person.
Learn more about VSS
Please use the following link to access our Diagnostic Criteria for Visual Snow Syndrome (to share with your doctor, etc.), as well as a more comprehensive list of symptoms with photo references.

Causes of VSS
The exact cause of VSS is still unknown. VSS patients have attributed the onset of their symptoms to a wide variety of potential causes, including medications, episodes of extreme physical or mental stress, concussion/TBI, migraine, infectious disease, surgery, and more. Although researchers have not identified a singular mechanism responsible for onset in all VSS cases, they have acquired valuable insights into its origins.
The first documented cases of visual snow/static vision were reported in the Transactions of the American Ophthalmological Society in 1944. Frank D. Carroll published descriptions of 6 patients experiencing visual disturbances induced by digitalis. Carroll surmised that digitalis impaired the central nervous system, stimulating the cerebrum to cause visual disturbances.
Today, the origin of VSS has been linked to hyperactivity in the visual cortex (lingual gyrus) of the brain, abnormalities in the visual processing centers of the brain, and alterations in the neural signals between the eyes and brain. Research has also demonstrated cortical hyper-reactivity in visual brain areas, indicating a network disorder rather than a focal pathology. Imaging studies (7-Tesla MRI and FDG-PET/MRI) have also shown microstructural and functional connectivity differences in cortical and thalamic regions. Possible biomarkers of VSS have been discovered: abnormalities in glutamatergic and serotoninergic neurotransmission.
In a recent groundbreaking study supported by the Visual Snow Initiative, researchers discovered the first-ever possible biological basis of VSS, revealing that the patterns of activity in two brain chemical systems, glutamate and serotonin, are different in people with VSS compared to those without the condition.
Researchers used a novel approach in the study, which combined information from positron emission tomography (PET) imaging on the distribution of different chemical receptors in the brain with functional Magnetic Resonance Imaging (fMRI) analysis. Using this Receptor-Enriched Analysis of Functional Connectivity by Targets (REACT) approach, researchers extract a map of activity of brain chemicals across the different brain areas.
The five brain chemicals examined in this study were noradrenaline, dopamine, serotonin, glutamate and gamma-aminobutyric acid (GABA). Researchers found that in patients with VSS, there were particular differences in the activity of glutamate and serotonin networks in specific areas of the brain.
There was less synchronized activity (or functional connectivity) in the glutamate networks in the anterior cingulate cortex (ACC) in those with VSS compared to healthy controls and those with migraine. The ACC is a hub for thinking and top- down control over sensory inputs. The different pattern of activity could represent an interruption in the filtering and integration of visual information.
Analysis also showed that VSS patients had reduced functional connectivity in the serotonin networks of the visual cortex, insula, temporal pole and orbitofrontal areas of the brains compared to healthy controls.
This reduced connectivity in serotonin networks was also seen in migraine patients with aura, suggesting a biological link between VSS and aura. The findings suggest that serotonin activity in VSS patients may be influencing the integration of complex sensory information. The results did not find any differences for the other brain chemicals that were investigated in the study.
Research into the causes of VSS, its pathophysiology, and further treatment options has made significant progress in recent years; it is ongoing and increasing day by day.
Latest News & Research
Here, our team will share the latest news and updates regarding the Visual Snow Initiative, research studies, interviews, projects, as well as any additional information related to our global efforts to better understand, treat, and/or cure Visual Snow Syndrome.
Diagnosing & Managing VSS
Historically, it has been challenging for people with VSS to receive an accurate diagnosis.
VSS is diagnosed based on a patient’s symptoms and a thorough clinical evaluation, including a comprehensive medical history and a comprehensive eye exam to rule out eye-related conditions. (Optometric and ophthalmological examinations typically yield “normal” results.) In some cases, an MRI or EEG may be ordered to rule out other neurological conditions. In addition to meeting the Diagnostic Criteria, VSS typically entails a diagnosis of exclusion.
Neuro-ophthalmologists and neurologists are best equipped to address VSS, including some ophthalmologists, optometrists, neuro-optometrists, and vision therapists who are trained in the management/treatment of VSS symptoms.
Based on the patient’s specific symptoms and medical history, managing VSS may require a multidisciplinary approach. Depending on which (visual and non-visual) symptoms they experience, doctors with expertise in the brain and/or eyes who treat associated symptoms may work independently or together. They can develop a safe and comprehensive plan that best addresses their patient’s needs, taking into account both the neurological and ocular aspects of VSS.
The types of physicians involved in VSS include:
- Neuro-ophthalmologist: Doctor with expertise in both neurology and ophthalmology, addressing visual issues linked to the nervous system
- Neurologist: Doctor specializing in the diagnosis and treatment of brain, spinal cord, and nervous system disorders
- Ophthalmologist: Doctor specializing in eye care, diagnosing and treating various eye conditions and performing surgeries
- Neuro-optometrist: Vision care professional trained in neurology and optometry, focusing on vision problems related to neurological conditions
- Optometrist: Vision care professional specializing in visual exams, corrective lenses, and managing common eye conditions
If you suspect you may have VSS, you can refer your doctor to our Diagnostic Criteria.
It can sometimes be difficult to find medical professionals who understand or specialize in VSS. VSI also has a list of physicians from around the world with knowledge of VSS that can help with diagnosis and treatment options. For more information, please see our Physicians & Specialists Directory.
As mentioned, VSS is a neurological disorder that impacts sensory processing, especially visual perception and the pathway between the brain and eyes; it involves complex interactions between the brain and the visual system. The condition may entail both visual and non-visual symptoms, many of which are associated with other medical conditions as well. Doctors with expertise in the brain and eyes can help patients with many of these symptoms, as they may already have experiencing treating them within their practice.
They are also able perform various assessments and diagnostic tests relevant to VSS. For example, a neurologist might conduct exams and imaging studies to evaluate brain function, while an ophthalmologist might perform eye exams and tests to assess visual function and eye health. Combining these assessments with communication and collaboration between the physicians involved can lead to an accurate diagnosis and effective plan for managing symptoms.

Support Visual Snow Syndrome Research
All donations to the Visual Snow Initiative go directly to Visual Snow Syndrome (VSS) research.
Your tax-deductible contribution ensures that global research will continue and makes a positive difference in the lives of people affected by VSS.