01.
Educate Yourself
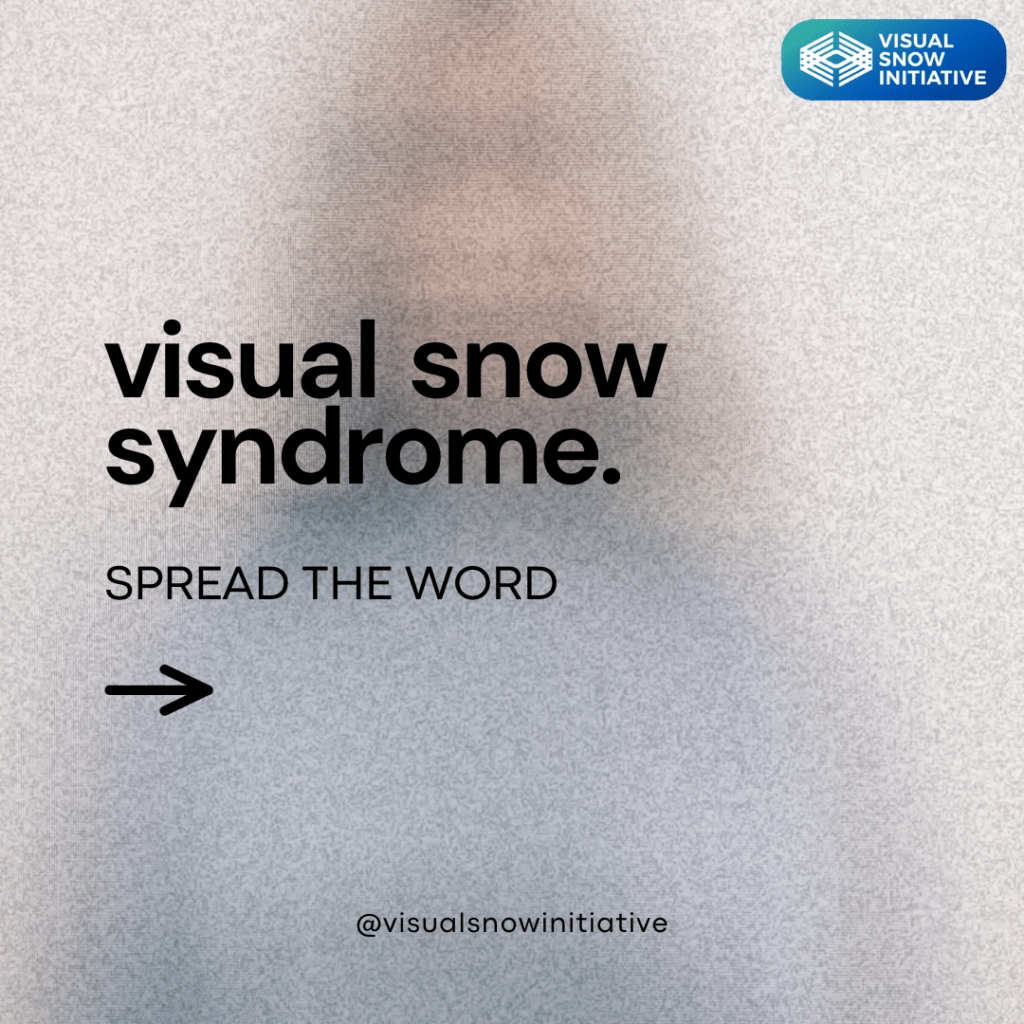
If you have recently been diagnosed with Visual Snow Syndrome (VSS), here is what you need to know:
Note: If you suspect you or a loved one may have VSS but have not received a diagnosis, please consult a qualified healthcare professional (such as a neuro-ophthalmologist or other physician within our directory) and show them the VSS Diagnostic Criteria.
After being diagnosed, take the time to understand what VSS is and how it may impact your quality of life. The information and resources available on the Visual Snow Initiative’s (VSI) website can help.
Learn about the following and view photo examples of:
- The visual and non-visual symptoms of VSS
- How VSS symptoms vary from person-to-person
- Ways that can help manage/treat your symptoms
- Progress in knowledge, research, and awareness
- VSI’s latest work and funded studies
- FAQs and more
Knowledge is power when it comes to understanding your condition and trying to communicate about VSS with physicians, family, and friends.