Researchers
Kenneth J. Ciuffreda, OD, Ph.D. Barry Tannen, OD M.H. Esther Han, OD SUNY/College of Optometry, Brain Injury Clinical Research Unit
Introduction
One of the most interesting and intriguing, as well as bothersome, visual abnormalities, is the presence of “visual snow” (VS), more specifically referred to as the “visual snow syndrome” (VSS).
These individuals perceive a somewhat pixelated visual world, sometimes fuzzy, with either black-and-white or chromatic dots appearing in a single plane in the foreground superimposed over the entire visual scene.
This is typically reported to be a constant, persistent phenomenon that has been present for years. They frequently describe it as being akin to the “snow” that is present when the primary television signal is reduced, and the residual electronic “noise” predominates on the screen.
In the present paper, several cases of VSS that the authors have examined will be discussed, as well as related information. The emphasis will be placed on the development of a comprehensive VSS patient diagnostic symptom survey, as well as discussion of the neuro-optometric treatment options that were successfully prescribed.
Discussion
The literature on VSS indicates that the VS per se is constantly present, once it initially becomes manifest, frequently at an early age (e.g., ages 11-14 years). Our small sample of individuals with VS (and VSS), which was obtained by “convenience sampling”, suggests otherwise with regards to constancy. Three of the ten (30%) reported their VS to be transient, and infrequent.
What might account for this discrepancy? We speculate that VS/ VSS may be more prevalent than currently believed. Some who noted VS at an early age either thought it was “normal” or were fearful that would be labelled as “crazy” or “weird”. Thus, while VS/VSS indeed may not be common, it may not be that rare, per our case scenarios.
Furthermore, in discussion with one experienced neuro-optometrist, he reported seeing 30-50 such patients per year.
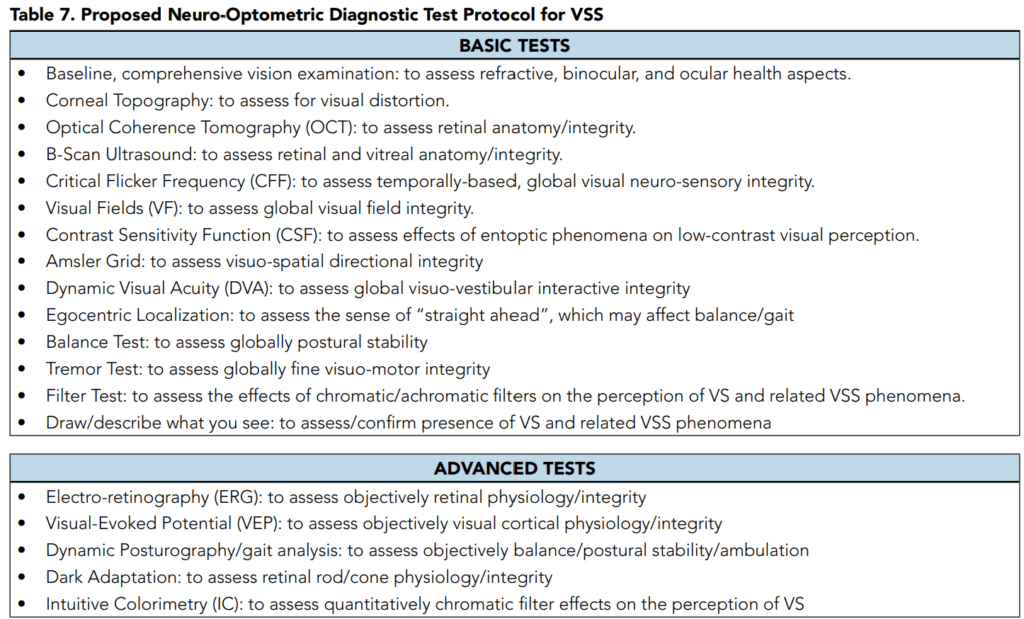
Thus, the neuro-optometrist and others in the field are encouraged to query in that direction at the slightest suspicion of VS/VSS to obtain the proper diagnosis. To this end, we have proposed a neuro-optometric, diagnostic, clinical test protocol for the patient with VSS based on the literature findings. Of particular interest to the neurooptometrist and others (e.g., vision therapist, occupational therapist) is the use of neuro-optometric rehabilitation (NORT) to reduce symptomatology in patients with VSS.
So far, there have been two primary optometric routes. The use of chromatic and achromatic filters show promise. In our limited experience, this has included the BPI-Omega, FL-41, and custom color filtration using the Intuitive Colorimeter, as well as achromatic gray tints.
Thus far, most of the chromatic tints have included a blue-blocking component (e.g., yellow). Their effectiveness may be due to a specific chromatic-based neurological mechanism, which remains unknown, and/or in part simply to luminance reduction which decreases the perceived intensity of the VS. We believe that both are involved. These arguments may also relate to the perception of the other visual symptoms. Our positive findings here are consistent with an earlier medically-based research study.
Read More Here